ABSTRACT
Background: We aimed to report our results of peri·navicular arthrodesis with autologous iliac bone graft for Stage III Müller Weiss disease. Methods: Nine cases of Stage III Müller·Weiss disease according to the Maceira classification (four male and five female) with average age of 48.2 (range, 41 to 58) years, had mild or severe midfoot pain with the longitudinal arch collapse. The patients, all of whom had failed conservative treatment for more than 6 months, underwent peri·navicular arthrodesis. All patients were followed up at 3, 6, 9, and 12 months, and then every 6 months with AOFAS ankle·hindfoot scores and radiographic measurements. Mean followup time for radiological and clinical evaluation was 22.4 (rangem 12 to 52) months. Results: All patients were satisfied with their clinical results without pain 12 months after surgery. The mean AOFAS ankle·hindfoot scores improved from 40.1 ± 8.3 preoperatively to 90.9 ± 2.1 at the last followup (p < 0.05). A solid fusion was found in all cases at 3 months after surgery by radiographic and clinical evaluation. The average longitudinal arch height increased from 46.1 ± 2.1 mm preoperatively to 53.5 ± 2.3 mm at the last followup (p < 0.05) on the lateral weightbearing radiograph. Conclusion: The peri·navicular arthrodesis with autologous iliac bone graft resulted in a good outcome for Stage III Müller·Weiss disease with good clinical outcomes, high fusion rate, and obvious improvement of the longitudinal arch height.
Level of Evidence: IV, Retrospective Case Series
Key Words: Müller-Weiss Disease; Autologous Bone Graft;Arthrodesis; Osteotomy; Internal Fixation
INTRODUCTION
Müller·Weiss disease (MWD) is a rarely diagnosed condition where the navicular undergoes spontaneous osteonecrosis in the adult.Maceira classified this disease into five stages according to the degree of the deformity based upon radiographs: (a) Stage I: minute changes that are visible only on nuclear bone scan or MRI; (b) Stage II: mild compression of the navicular visible on plain radiographs(c) Stage III: increased compression of the navicular with bony fragmentation and lowering of the longitudinal arch(d) Stage IV: increased fragmentation of the navicular where longitudinal arch collapses; and (e) Stage V: complete extrusion of the navicular with the talus articulating with the medial cuneiform. Therefore, the key goals of treatment are both pain relief and recovery of the longitudinal arch height.Several surgical techniques were reported to treat this disease including: (1) internal fixation of the navicular,(2) talonavicular arthrodesis, (3) triple arthrodesis, and (4) talonavicular-cuneiform (TNC) arthrodesis.Internal fixation of the navicular is considered to be a good choice in some acute fractures of the navicular, but in MWD there is a lack of bone stock to perform it satisfactorily and the bone is necrotic. Isolated talonavicular arthrodesis does not resolve the joint incongruence that is present in the naviculocuneiform joints and often leads to pseudarthrosis.Although triple arthrodesis could optimize consolidation,it does not resolve the problem in the naviculocuneiform joints. In fact, we believe talonavicular·cuneiform arthrodesis is more advantageous in MWD since it can address the incongruence at both the TNC and talonavicular joints resulting in pain alleviation and excellent consolidation. Hence, in the current study, we report a modification of the previous technique of peri·navicular arthrodesis for Stage III MWD and analyze the clinical outcomes.
MATERIALS AND METHODS
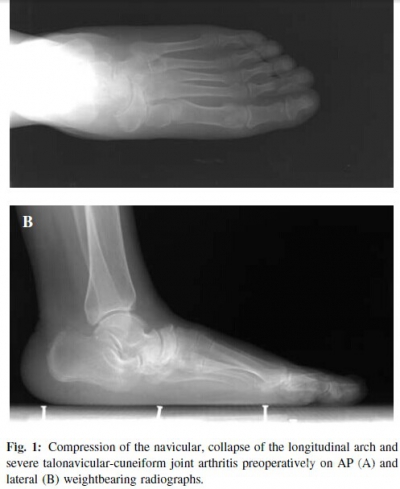
In the absence of a satisfactory response to conservative measures for more than 6 months, nine Stage III MWD patients (four male and five female), with an average age of 48.2 (range, 41 to 58) years, underwent perinavicular arthrodesis with reverse “V”shaped osteotomy and autologous iliac bone graft between 2006 and 2008. The mean followup time for radiological and clinical evaluation was 22.4 (range, 12 to 52) months. All patients complained of midfoot pain on standing and walking and had gradual collapse of the medical longitudinal arch without history of trauma or glucocorticoid use or secondary osteonecrosis from rheumatoid arthritis, diabetes, tuberculosis, etc. The compression of the navicular, collapse of the medical longitudinal arch and severe talonavicular·cuneiform joint arthritis were found in all cases on radiography (Figure 1).
Surgical technique
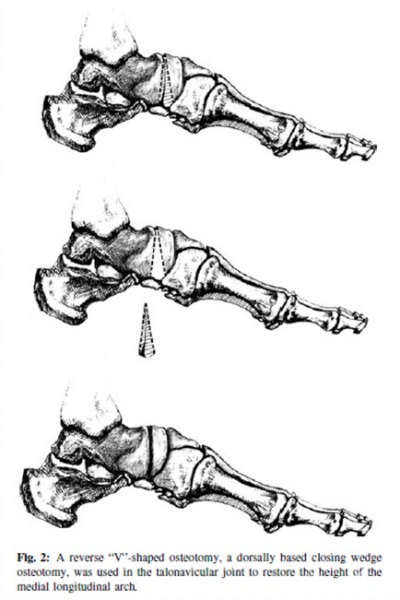
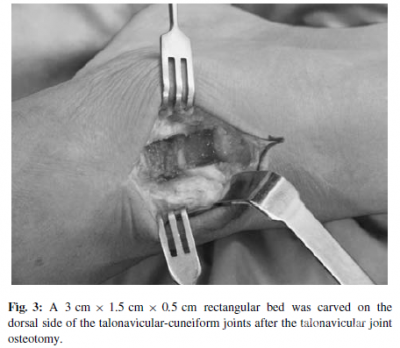
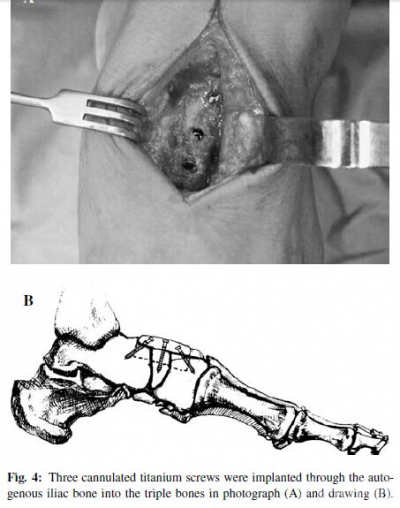
All procedures were performed in the supine position after satisfactory spinal anesthesia with a tourniquet. The navicular, cuneiforms, and head of the talus were exposed through a dorsal incision (about 5cm) between the anterior tibial tendon and the extensor hallucis longus. After removing the cartilage of the talonavicular-cuneiform articular surfaces, a reverse “V”shaped osteotomy, which was a dorsal closing wedge osteotomy, was performed through the talonavicular joint to restore the height of medial longitudinal arch (Figure 2). A rectangular bed (about 3cm×1.5cm×0.5cm) was made from the talus to the cuneiforms on the dorsal side of the talonavicular·cuneiform joints with an oscillating saw and osteotome (Figure 3). A tricortical autogenous graft of the same size and shape was obtained from the iliac crest and inserted in the bed with the aid of plantarflexion of the foot. Three cannulated 4.0mm titanium screws (Newdeal,USA) were implanted through the autogenous iliac bone into the talus, navicular and the first cuneiform across the talonavicular·cuneiform fusion interface (Figure 4). Fluoroscopic control was used throughout to ensure optimal placement of the hardware.
Postoperative management and evaluation
Patients were immobilized in a cast for 6 weeks. The patient began to walk with a crutch with partial weightbearing 6 weeks after surgery, and with full weightbearing 3 months after surgery which depended upon bone fusion by radiograph.
All patients were evaluated preoperatively, postoperatively at 3, 6, 9, 12 months, and then every 6 months by clinical examination, AOFAS ankle·hindfoot score, and radiographic measurements from weightbearing radiographs of the feet.
The fusion was considered to be successful when trabeculation was seen to cross the fusion site in the radiographs. MRI scans were used to assess the destruction of talonavicularcuneiform joints preoperatively. Onset of deformity and complications in or after surgery were recorded exactly. The weightbearing AP and lateral view were used to evaluate deformity and longitudinal arch height from a distance from a point midway between anterior and posterior margins of dorsal navicular and a line connecting the plantar calcaneus and plantar first metatarsal head. Statistical analysis All the data were treated with SPSS 13.0 software,independent sample paired t-test, and statistical significance was defined as p < 0.05.
RESULTS
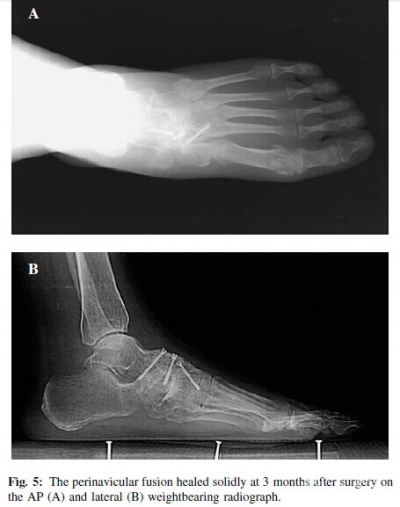
At the last followup, all feet were pain·free, and the deformity was also corrected satisfactorily without any surgical complication including infection, skin necrosis, and nerve injury. There was no case of persistent graft donor site pain at the hip. The average AOFAS ankle·hindfoot score was improved from 40.1±8.3 preoperatively to 90.9±2.1 at the last followup (p = 0.0004).Radiographically, all the feet fused solidly at 3 months after surgery without screw breakage or loosening (Figure 5).The foot appearance improved with normal longitudinal arch height on the lateral view (Figure 6). The average longitudinal arch height increased from 46.1± 2.1mm preoperatively to 53.5±2.3 mm at the last followup (p < 0.05) on the lateral weightbearing radiograph.
DISCUSSION
MWD is a rare pathological condition in adults.Most of the patients complain of long·standing mechanical pain on the dorsum of feet, caused by the perinavicular osteoarthritic changes and arch collapse. This diease was classified into five stages according to the degree of the deformity by Maceira.In the early stages, conservative treatment with rest, physical therapy and NSAIDs can be effective for alleviating the pain, but with no ability to stop the progression of the disease. Surgical treatment should be considered for failure of conservative treatment or severe deformity of the foot. Several surgical treatments have been proposed to correct the deformity and alleviate the pain;however, no technique can be considered the gold standard.Arthrodesis is advocated by most for the Stage III cases, including talonavicular arthrodesis, triple arthrodesis or talonavicular·cuneiform (TNC) arthrodesis, which is called peri·navicular arthrodesis. Both isolated talonavicular arthrodesis and triple arthrodesis do not resolve the problem in the naviculocuneiform joints,thus we advocate the perinavicular arthrodesis for the Stage III MWD.
The perinavicular arthrodesis can be performed through a medial or dorsal approach. The dorsal approach, used in this group of patients, allowed easy exposure of the navicular, cuneiforms, and head of the talus while avoiding neurovascular structures. According to Watson·Jones,a trapezoidal bed can be carved on the navicular from the talus to the cuneiforms. A tricortical autogenous graft of this shape was obtained from the iliac crest and inserted in the bed with the aid of plantarflexion of the foot. Meanwhile,if the steps were performed carefully, as Watson-Jones described, osteosynthesis devices were unnecessary because the graft entered in a self-locking receptor bed. However,we felt it was not a stable fixation for arthrodesis.In this group, we used a rectangle bed (more easily carved than the trapezoidal bed as well as a tricortical autogenous graft. In addition, to prevent potential non·union, three cannulated titanium 4.0mm screws were implanted through the tricortical autogenous. Postoperatively, all the feet fused solidly at 3 months after surgery without screw breakage or looseness.
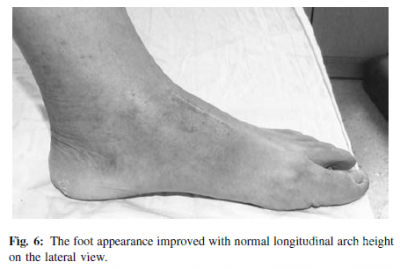
In our series, the longitudinal arch height also improved in all patients with an increase from 46.1±2.1 mm preoperatively to 53.5 ± 2.3 mm. In this procedure, the reverse“V”shaped osteotomy of the talonavicular joint helped increase the longitudinal arch height. The tricortical graft,which was inserted in the rectangle bed, may have lengthened the dorsal surface of the midfoot thus increasing the longitudinal arch height.
All patients were satisfied with their clinical results,namely free of pain with improved deformity.We also did not encounter any complication or infection in this group,which has been observed in the other study.
CONCLUSION
The perinavicular arthrodesis with a reverse “V”shaped osteotomy and autologous iliac bone graft was a good alternative for Stage III MWD, with good clinical outcomes,high fusion rate and obvious improvement of the longitudinal arch height.
转载于American Orthopaedic Foot & Ankle Society
参考文献(略)
作者 Hong-Hui Cao, MD; Kang-LaiTang, MD, PhD; Jian-Zhong Xu, MD, PhD