张卫国/田康团队在OJSM发表髋关节镜下盂唇修复入路选择策略最新研究
作者:张卫国,田康
来源:大连医科大学附属第一医院关节与运动医学科
近日,大连医科大学附属第一医院关节与运动医学科张卫国教授、田康教授团队研究成果在The Orthopaedic Journal of Sports Medicine发表。文章标题为《髋关节镜下盂唇修复中缝合锚钉置入的入路选择:基于三维模型重建的研究》(Portal Selection for Suture Anchor Placement During Hip Arthroscopic Labral Repair:A Study Based on 3-Dimensional Model Reconstruction),研究对目前常用的髋关节镜入路进行了安全性评价,并提出了内移中前入路以改善髋臼前方锚钉置入的安全性。
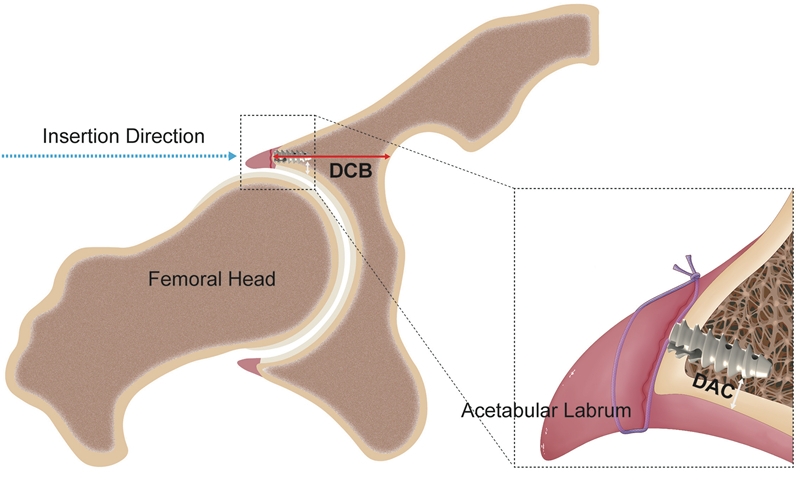
研究利用CT影像资料重建20例髋关节的三维模型,计算机模拟髋关节镜下缝合锚钉置入过程。通过锚钉与关节软骨距离(the distances from the anchor to the articular cartilage,DAC)和锚钉置入点到皮质骨距离(the distances from the acetabular insertion point to the cortical bone,DCB)定量评价髋关节镜入路在髋臼前方4点至后方8点放置缝合锚钉的安全性。
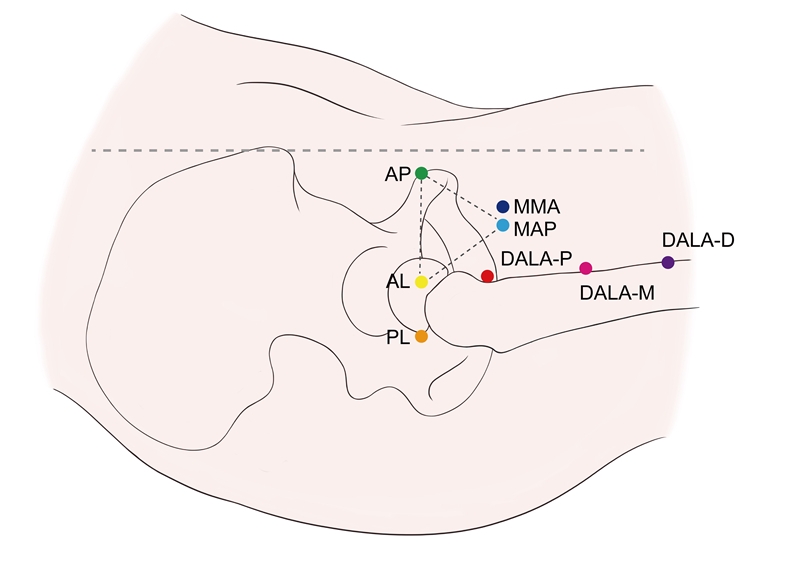
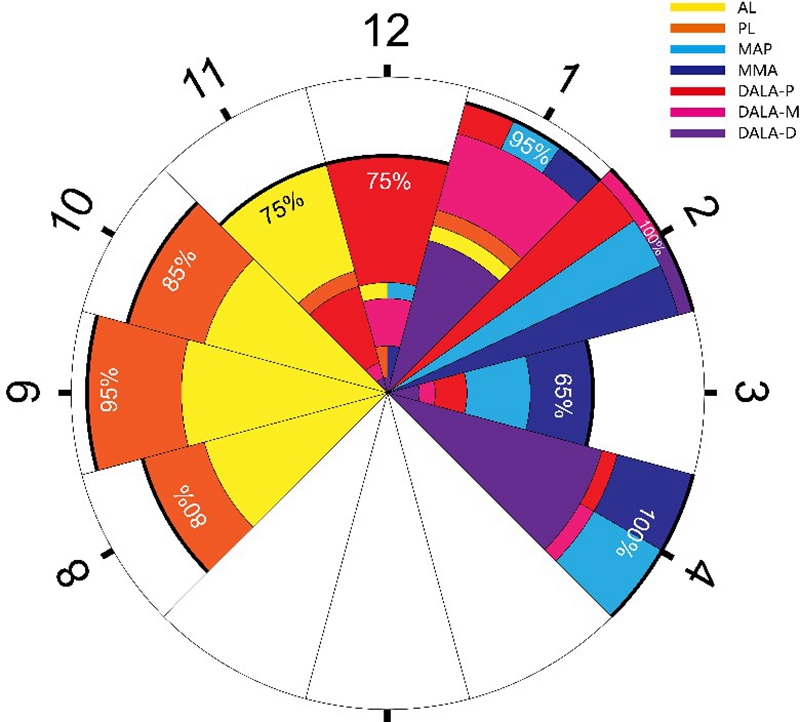
研究中不仅包含了常用的前外入路(anterolateral portal,AL)、后外入路(posterolateral portal,PL)、中前入路(midanterior portal,MAP)和由近及远的三个远前外辅助入路(distal anterolateral accessory portals,DALA),分别是近端DALA(DALA-P)、中间DALA(DALA-M)和远端DALA(DALA-D)。此外,研究中提出了内移中前入路(medial midanterior portal, MMA)以改善前方髋臼放置缝合锚钉的安全性。
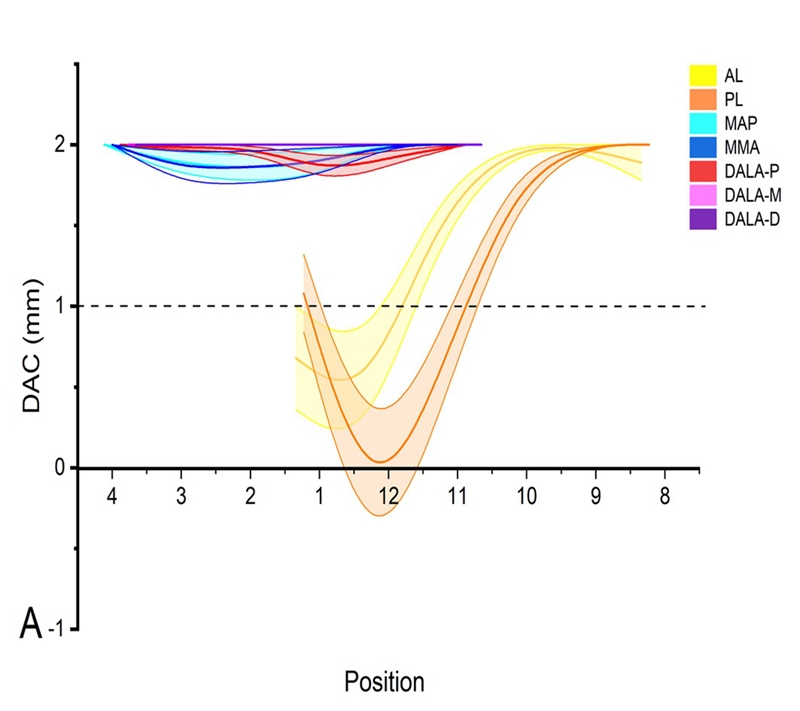
研究发现经AL入路进行缝合锚钉置入时,在1 点钟位置(0.68±0.32mm;P<.001)和12点钟位置(0.37±0.30mm;P<.001)具有较小的DAC;经PL入路进行缝合锚钉置入时,在12 点钟位置(-0.35±0.38mm;P <.001)和11点钟位置(0.60±0.24mm;P<.001)具有较小的DAC,更容易发生髋关节软骨损伤(articular cartilage violation,ACV)。
另一方面,研究发现某些入路在放置缝合锚钉时具有较小的DCB, 更容易发生髋关节皮质穿透(cortical bone penetration,CBP)。他们分别是DALA-P入路在3点位置(8.93±2.12mm;P<.001)和11点位置(9.59±2.84mm;P<.001),MAP入路在12点位置(13.76±3.89mm;P<.001)和11点位置(0.27±0.27)mm;P<.001), MMA入路在12点位置(5.96±2.31mm;P<.001)和11点位置(0mm;P<.001)。
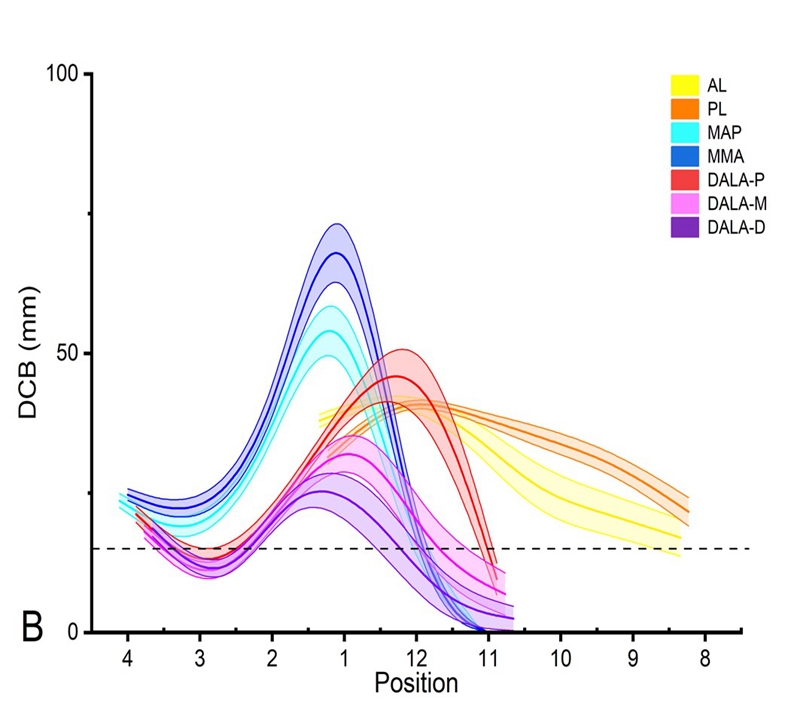
最后,锚钉安全放置结果显示MAP在4点、2点和1点成功率较高,MMA在4点、3点、2点和1点成功率较高,DALA-P在2点、1点和12点成功率较高,AL在11点成功率较高,PL在10点、9点和8点成功率较高。髋臼不同位置的盂唇撕裂可以通过选择合适的入路,提高缝合锚钉放置的安全性。值得注意的是以往入路在前方3点放置锚钉成功率未能令人满意,在此置入缝合锚钉需更加注意。研究中提出的MMA入路有助于提高此处锚钉放置的安全性。
该研究利用髋关节三维模型对常用髋关节镜入路放置缝合锚钉的安全性进行了评价,指出髋臼不同位置盂唇损伤修复时较为合适的入路。此外,研究提出了MMA入路以改善髋臼前方放置锚钉的安全性,为髋关节镜下盂唇修复的入路选择提供了新的参考和思路。
点击查看原文:
参考文献:
1. Blankenbaker DG, De Smet AA, Keene JS, Fine JP. Classification and localization of acetabular labral tears. Skeletal Radiol. 2007;36(5):391-397.
2. Byrd JWT, Jones KS, Loring CL, Sparks SL. Acetabular All-Suture Anchor for Labral Repair: Incidence of Intraoperative Failure due to Pullout. Arthroscopy. 2018;34(4):1213-1216.
3. Degen RM, O'Sullivan E, Sink EL, Kelly BT. Psoas tunnel perforation-an unreported complication of hip arthroscopy. J Hip Preserv Surg. 2015;2(3):272-279.
4. Degen RM, Poultsides L, Mayer SW, et al. Safety of Hip Anchor Insertion From the Midanterior and Distal Anterolateral Portals With a Straight Drill Guide: A Cadaveric Study. Am J Sports Med. 2017;45(3):627-635.
5. Douglass NP, Behn AW, Safran MR. Cyclic and Load to Failure Properties of All-Suture Anchors in Synthetic Acetabular and Glenoid Cancellous Bone. Arthroscopy. 2017;33(5):977-985 e975.
6. Dumont GD, Money AJ, Thier ZT. Acetabular Subchondral and Cortical Perforation During Labral Repair With Suture Anchors: Influence of Portal Location, Curved Versus Straight Drill Guides, and Drill Starting Point. Arthroscopy. 2019;35(8):2349-2354.
7. Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88(5):925-935.
8. Foster AD, Ryan J, Ellis T, Flom J. Safe suture anchor insertion for anterior and posterior hip labral repair. J Hip Preserv Surg. 2015;2(2):170-174.
9. Fry R, Domb B. Labral base refixation in the hip: rationale and technique for an anatomic approach to labral repair. Arthroscopy. 2010;26(9 Suppl):S81-89.
10. Groh MM, Herrera J. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med. 2009;2(2):105-117.
11. Hernandez JD, McGrath BE. Safe angle for suture anchor insertion during acetabular labral repair. Arthroscopy. 2008;24(12):1390-1394.
12. Ismailoglu AV, Ozdogmus O, Karaman MI, Kayaalp A, Kocaoglu B. Perpendicular drill bit alignment provides a practical guidance to determine the appropriate suture anchor insertion angle during acetabular labral repair. J Hip Preserv Surg. 2021;8(2):185-191.
13. Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21(12):1496-1504.
14. Kohnlein W, Ganz R, Impellizzeri FM, Leunig M. Acetabular morphology: implications for joint-preserving surgery. Clin Orthop Relat Res. 2009;467(3):682-691.
15. Larson CM, Dean RS, McGaver RS, Seiffert KJ, Giveans MR. Arthroscopic Debridement Versus Refixation of the Acetabular Labrum Associated With Femoroacetabular Impingement: Updated Mean 7-Year Follow-up. Am J Sports Med. 2022;50(3):731-738.
16. Lertwanich P, Ejnisman L, Torry MR, Giphart JE, Philippon MJ. Defining a safety margin for labral suture anchor insertion using the acetabular rim angle. Am J Sports Med. 2011;39 Suppl:111S-116S.
17. Lewis CL, Sahrmann SA. Acetabular labral tears. Phys Ther. 2006;86(1):110-121.
18. Maldonado DR, Monahan PF, Domb BG. Restoration of Labral Function in Primary Hip Arthroscopy From Labral Repair to Labral Reconstruction. Arthroscopy. 2021;37(10):3013-3015.
19. McGovern RP, Christoforetti JJ, Kivlan BR, et al. Allocation of Anchors During Labral Repair: A Multicenter Cohort Analysis of Labral Treatment in Hip Arthroscopy. Orthop J Sports Med. 2021;9(2):2325967120981983.
20. Nho SJ, Freedman RL, Federer AE, et al. Computed tomographic analysis of curved and straight guides for placement of suture anchors for acetabular labral refixation. Arthroscopy. 2013;29(10):1623-1627.
21. Philippon MJ, Schroder e Souza BG, Briggs KK. Labrum: resection, repair and reconstruction sports medicine and arthroscopy review. Sports Med Arthrosc Rev. 2010;18(2):76-82.
22. Robertson WJ, Kelly BT. The safe zone for hip arthroscopy: a cadaveric assessment of central, peripheral, and lateral compartment portal placement. Arthroscopy. 2008;24(9):1019-1026.
23. Shah A, Kay J, Memon M, et al. What Makes Suture Anchor Use Safe in Hip Arthroscopy? A Systematic Review of Techniques and Safety Profile. Arthroscopy. 2019;35(4):1280-1293 e1281.
24. Stanton M, Banffy M. Safe Angle of Anchor Insertion for Labral Repair During Hip Arthroscopy. Arthroscopy. 2016;32(9):1793-1797.
25. Suppauksorn S, Beck EC, Chahla J, et al. Comparison of Suction Seal and Contact Pressures Between 270 degrees Labral Reconstruction, Labral Repair, and the Intact Labrum. Arthroscopy. 2020;36(9):2433-2442.
26. Vandenbussche E, Saffarini M, Taillieu F, Mutschler C. The asymmetric profile of the acetabulum. Clin Orthop Relat Res. 2008;466(2):417-423.
作者简介

张卫国
二级教授,博士研究生导师,国务院特殊津贴专家,辽宁省特聘教授,辽宁省优秀专家,辽宁省名医。
学术任职:中国老年学和老年医学会老年运动医学分会副主任委,中华医学会骨科分会关节外科学组委员,辽宁省医学会骨科分会副主任委员,辽宁省医院协会副会长,大连市医学会运动医学分会主任委员。
科研方向:主要研究方向为骨关节退行性疾病、股骨头坏死、关节运动损伤等。主持国家课级题2项,辽宁省课题3项,荣获省科技进步奖一等奖1项、二等奖4项,三等奖1项,市科技进步一等奖1项、二等奖1项;发表学术论文40余篇,SCI收录22篇。从医执教30年,指导培养硕士生50余人,博士研究生12人。
田康
医学博士,副教授,硕士研究生导师,辽宁省“百千万”人才。
学术任职:中国医师协会运动医学医师分会青年委员,中华预防医学会骨与关节疾病预防控制专业委员会委员,中国医药教育协会科普健康教育工作委员会委员,辽宁省医学会运动医疗分会委员,大连市医学会运动医疗分会秘书,大连市骨科临床质控中心秘书
科研成果:主持关节软骨损伤修复领域国家自然科学基金1项、辽宁省自然科学基金面上项目1项。发表关节外科领域SCI文章7篇,参编关节外科译著3部,申请专利2项。在关节软骨损伤、自体软骨细胞移植修复领域主持并参与多项临床及基础研究。